Colorectal cancer prevention by diet (AKA the most important page on EatWell.MD)
Granted, as a gastroenterologist I firmly believe in the importance of screening or surveillance* colonoscopies to remove polyps and to prevent colorectal cancer (surveillance means the repeat scope you get if you’ve previously had polyps or have inflammatory bowel disease). However, a mind blowing presentation by Lawrence H. Kushi, Sc.D. (Director of Scientific Policy, Division of Research, Kaiser Permanente Northern California, Oakland CA) at the International Conference on Nutrition in Medicine in August 2018 redirected and strengthened my post polypectomy dietary advice to my patients.

The International Agency for Research on Cancer (IARC), the cancer agency of the World Health Organization has classified processed meat as carcinogenic to humans (Group 1), based on sufficient evidence in humans that the consumption of processed meat causes colorectal cancer. The experts concluded that each 50 gram portion (slightly less than the size of one ‘large’ egg) of processed meat eaten daily (hot dogs, bologna, ham, sausage, corned beef, beef jerky, or canned meat) increases your risk of colorectal cancer by 18%. You can find their release here:https://www.iarc.fr/wp-content/uploads/2018/07/pr240_E.pdf Group 1 carcinogens means that processed red meat shares the same category of certainty as asbestos, tobacco and ionizing radiation. This should rock your world…it pushed me further toward a WFPB diet for myself and my patients.

Consumption of red meat was classified as ‘probably’ carcinogenic to humans (Group 2A), based on limited evidence that the consumption of red meat causes cancer in humans and strong mechanistic evidence supporting a carcinogenic effect.This association was observed mainly for colorectal cancer, but associations were also seen for pancreatic cancer and prostate cancer. Group 2A carcinogens means that red meat shares the same category as acrylamide (the stuff in plastics), styrene (also stuff in plastics), and UV radiation. If you’ve abandoned your plastic water bottle and plastic food storage containers, reducing or eliminating red meat carries the same scientific weight.
The entire report can be seen here: http://www.thelancet.com/retrieve/pii/S1470204515004441
Carcinogenicity of consumption of red and processed meat. Véronique Bouvard, Dana Loomis, Kathryn Z Guyton et al. The Lancet Oncology VOLUME 16, ISSUE 16, P1599-1600, DECEMBER 01, 2015 Published:October 26, 2015DOI:https://doi.org/10.1016/S1470-2045(15)00444-1
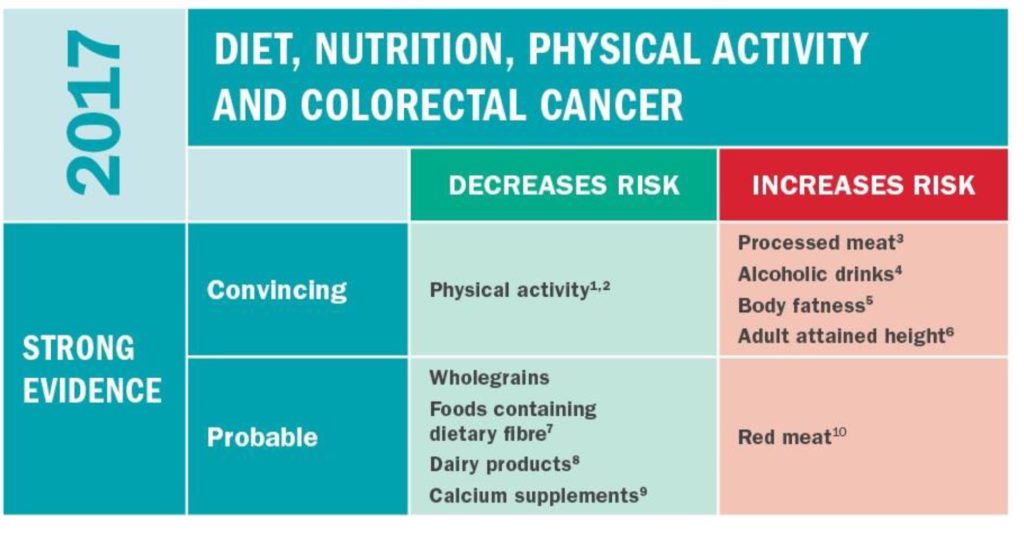
So beyond getting rid of processed red meats and red meats from your diet and getting your colonoscopy, what other dietary and environmental changes can you make to reduce your colorectal cancer risk? Note that this page will be fluid, changing and growing with additional scientific evidence.

Increase Exercise
Increase Fruits & vegetables
Increase Whole grains/Fiber
Reduce processed foods
Reduce alcohol consumption
Exercise
Med Sci Sports Exerc. 2019 Jun;51(6):1252-1261. doi: 10.1249/MSS.0000000000001937.
Physical Activity in Cancer Prevention and Survival: A Systematic Review.
McTiernan A1,2, Friedenreich CM3,4,5, Katzmarzyk PT6, Powell KE7, Macko R8, Buchner D9, Pescatello LS10, Bloodgood B11, Tennant B11, Vaux-Bjerke A12, George SM13, Troiano RP14, Piercy KL12; 2018 PHYSICAL ACTIVITY GUIDELINES ADVISORY COMMITTEE*.
https://www.ncbi.nlm.nih.gov/pubmed/31095082
PURPOSE:
This article reviews and updates the evidence on the associations between physical activity and risk for cancer, and for mortality in persons with cancer, as presented in the 2018 Physical Activity Guidelines Advisory Committee Scientific Report.
METHODS:
Systematic reviews of meta-analyses, systematic reviews, and pooled analyses were conducted through December 2016. An updated systematic review of such reports plus original research through February 2018 was conducted. This article also identifies future research needs.
RESULTS:
In reviewing 45 reports comprising hundreds of epidemiologic studies with several million study participants, the report found strong evidence for an association between highest versus lowest physical activity levels and reduced risks of bladder, breast, colon, endometrial, esophageal adenocarcinoma, renal, and gastric cancers. Relative risk reductions ranged from approximately 10% to 20%. Based on 18 systematic reviews and meta-analyses, the report also found moderate or limited associations between greater amounts of physical activity and decreased all-cause and cancer-specific mortality in individuals with a diagnosis of breast, colorectal, or prostate cancer, with relative risk reductions ranging almost up to 40% to 50%. The updated search, with five meta-analyses and 25 source articles reviewed, confirmed these findings.
CONCLUSIONS:
Levels of physical activity recommended in the 2018 Guidelines are associated with reduced risk and improved survival for several cancers. More research is needed to determine the associations between physical activity and incidence for less common cancers and associations with survival for other cancers. Future studies of cancer incidence and mortality should consider these associations for population subgroups, to determine dose-response relationships between physical activity and cancer risk and prognosis, and to establish mechanisms to explain these associations.
Fruits and vegetables
Antioxidants (Basel). 2019 May 18;8(5). pii: E137. doi: 10.3390/antiox8050137.
Dietary Flavonoids as Cancer Chemopreventive Agents: An Updated Review of Human Studies.
Rodríguez-García C1,2, Sánchez-Quesada C3,4,5, J Gaforio J6,7,8,9.
https://www.ncbi.nlm.nih.gov/pubmed/31109072
Over the past few years, interest in health research has increased, making improved health a global goal for 2030. The purpose of such research is to ensure healthy lives and promote wellbeing across individuals of all ages. It has been shown that nutrition plays a key role in the prevention of some chronic diseases such as obesity, cardiovascular disease, diabetes, and cancer. One of the aspects that characterises a healthy diet is a high intake of vegetables and fruits, as both are flavonoid-rich foods. Flavonoids are one of the main subclasses of dietary polyphenols and possess strong antioxidant activity and anti-carcinogenic properties. Moreover, some population-based studies have described a relationship between cancer risk and dietary flavonoid intake. In this context, the goal of this review was to provide an updated evaluation of the association between the risk of different types of cancers and dietary flavonoid intake. We analyzed all relevant epidemiological studies from January 2008 to March 2019 using the PUBMED and Web of Science databases. In summary, this review concludes that dietary flavonoid intake is associated with a reduced risk of different types of cancer, such as gastric, breast, prostate, and colorectal cancers.
Prev Med. 2019 May;122:20-30. doi: 10.1016/j.ypmed.2019.03.013.
Estimates of the current and future burden of cancer attributable to low fruit and vegetable consumption in Canada.
Poirier AE1, Ruan Y2, Hebert LA2, Grevers X2, Walter SD3, Villeneuve PJ4, Brenner DR5, Friedenreich CM6; ComPARe Study Team.
https://www.ncbi.nlm.nih.gov/pubmed/31078169
Low fruit and vegetable consumption is associated with colorectal cancer and may be associated with lung, breast, bladder, pancreatic, ovarian, liver, stomach, esophageal, head and neck cancers. We estimated the current attributable and future avoidable burden of cancer associated with low fruit and vegetable consumption in Canada. Using data on cancer incidence, exposure prevalence and risk effects, we estimated the population attributable risk (PAR) for cancers associated with low fruit and vegetable consumption as well as the future avoidable burden. The prevalence of fruit and vegetable consumption was projected to 2032 and cancer incidence was projected to 2042 to estimate the future potential impact fraction of cancer attributable to low fruit and vegetable consumption. Based on estimates from the Canadian Community Health Survey, the prevalence of low fruit (<4 servings/day) and vegetable (<4 servings/day) consumption in the Canadian population was 80.5% and 86.6%, respectively. The PARs for colorectal cancer associated with low fruit and vegetable consumption were 6.1% (1, 371 cases) and 2.2% (487 cases), respectively. For all incident cancers in 2015, 0.7% and 0.3% were attributable to low fruit and vegetable consumption, respectively. An increase of one serving/week of fruit could prevent 20,710 colorectal cancer cases cumulatively by 2042, and the same increase in vegetable consumption could prevent 10,185 cases. Although more research on the association between fruit and vegetable consumption and cancer risk is needed, our results demonstrate that with reasonable increases in current fruit and vegetable consumption by Canadians, over 30,000 colorectal cancer cases could be prevented by 2042.
Whole grains/Fiber
Int J Cancer. 2019 May 1. doi: 10.1002/ijc.32382. [Epub ahead of print]
Dietary intake of fiber, whole grains and risk of colorectal cancer: An updated analysis according to food sources, tumor location and molecular subtypes in two large US cohorts.
He X1,2,3, Wu K4, Zhang X5, Nishihara R4,6,7,8,9, Cao Y10, Fuchs CS11, Giovannucci EL4,5,8, Ogino S6,7,8,12,13, Chan AT2,3,5,13,14, Song M2,3,4,8.
https://www.ncbi.nlm.nih.gov/pubmed/31044426
Epidemiologic evidence relating fiber intake to colorectal cancer (CRC) remains inconclusive and data are limited on different food sources of fiber and heterogeneity by tumor subsite and molecular profile. We prospectively followed for CRC incidence 90,869 women from the Nurses’ Health Study (1980-2012) and 47,924 men from the Health Professionals Follow-up Study (1986-2012), who completed a validated food frequency questionnaire every 4 years. Cox proportional hazards regression was used to examine the associations with CRC risk for total, cereal, fruit and vegetable fiber and whole grains. We also assessed the associations according to tumor subsites (proximal colon, distal colon and rectum) and molecular markers (microsatellite instability, BRAF mutation, CpG island methylator phenotype and KRAS mutation). We documented 3,178 CRC cases during 3,685,903 person-years of follow-up in the NHS and HPFS. Intake of total dietary fiber was not associated with CRC risk after multivariable adjustment in either women (hazard ratio [HR] comparing extreme deciles, 1.17; 95% CI, 0.92-1.48, ptrend = 0.55) or men (HR, 0.90; 95% CI, 0.67-1.21, ptrend = 0.47). Higher intake of cereal fiber and whole grains was associated with lower CRC risk in men with an HR of 0.75 (95% CI, 0.57-1.00) and 0.72 (95% CI, 0.54-0.96), respectively. No heterogeneity was detected by tumor subsite or molecular markers (pheterogeneity > 0.05). Higher intake of total dietary fiber within the range of a typical American diet is unlikely to substantially reduce CRC risk. The potential benefit of cereal fiber and whole grains in men warrants further confirmation.
Int J Epidemiol. 2019 Apr 17. pii: dyz064. doi: 10.1093/ije/dyz064. [Epub ahead of print]
Diet and colorectal cancer in UK Biobank: a prospective study.
Bradbury KE1,2, Murphy N3, Key TJ1.
https://www.ncbi.nlm.nih.gov/pubmed/30993317
BACKGROUND:
Most of the previous studies on diet and colorectal cancer were based on diets consumed during the 1990s.
METHODS:
We used Cox-regression models to estimate adjusted hazard ratios for colorectal cancer by dietary factors in the UK Biobank study. Men and women aged 40-69 years at recruitment (2006-10) reported their diet on a short food-frequency questionnaire (n = 475 581). Dietary intakes were re-measured in a large sub-sample (n = 175 402) who completed an online 24-hour dietary assessment during follow-up. Trends in risk across the baseline categories were calculated by assigning re-measured intakes to allow for measurement error and changes in intake over time.
RESULTS:
During an average of 5.7 years of follow-up, 2609 cases of colorectal cancer occurred. Participants who reported consuming an average of 76 g/day of red and processed meat compared with 21 g/day had a 20% [95% confidence interval (CI): 4-37] higher risk of colorectal cancer. Participants in the highest fifth of intake of fibre from bread and breakfast cereals had a 14% (95% CI: 2-24) lower risk of colorectal cancer. Alcohol was associated with an 8% (95% CI: 4-12) higher risk per 10 g/day higher intake. Fish, poultry, cheese, fruit, vegetables, tea and coffee were not associated with colorectal-cancer risk.
CONCLUSIONS:
Consumption of red and processed meat at an average level of 76 g/d that meets the current UK government recommendation (≤90 g/day) was associated with an increased risk of colorectal cancer. Alcohol was also associated with an increased risk of colorectal cancer, whereas fibre from bread and breakfast cereals was associated with a reduced risk.
Reduce processed foods
Int J Mol Sci. 2019 Apr 25;20(8). pii: E2051. doi: 10.3390/ijms20082051.
Xenobiotics Formed during Food Processing: Their Relation with the Intestinal Microbiota and Colorectal Cancer.
Nogacka AM1,2, Gómez-Martín M3,4, Suárez A5,6, González-Bernardo O7, de Los Reyes-Gavilán CG8,9, González S10,11.
https://www.ncbi.nlm.nih.gov/pubmed/31027304
The colonic epithelium is exposed to a mixture of compounds through diet, among which some are procarcinogens, whereas others have a protective effect. Therefore, the net impact of these compounds on human health depends on the overall balance between all factors involved. Strong scientific evidence has demonstrated the relationship between nitrosamines (NA), heterocyclic amines (HCAs), and polycyclic aromatic hydrocarbons (PAHs), which are the major genotoxins derived from cooking and food processing, and cancer. The mechanisms of the relationship between dietary toxic xenobiotics and cancer risk are not yet well understood, but it has been suggested that differences in dietary habits affect the colonic environment by increasing or decreasing the exposure to mutagens directly and indirectly through changes in the composition and activity of the gut microbiota. Several changes in the proportions of specific microbial groups have been proposed as risk factors for the development of neoplastic lesions and the enrichment of enterotoxigenic microbial strains in stool. In addition, changes in the gut microbiota composition and activity promoted by diet may modify the faecal genotoxicity/cytotoxicity, which can be associated with a higher or lower risk of developing cancer. Therefore, the interaction between dietary components and intestinal bacteria may be a modifiable factor for the development of colorectal cancer in humans and deserves more attention in the near future.

